Frozen Shoulder and Menopause: Causes, Symptoms, and Solutions
Nov 19, 2024
Menopause is a natural transition that brings about various physical and hormonal changes in a woman's body. One of the lesser-known conditions that can arise during this phase is frozen shoulder, also known as adhesive capsulitis. This condition can cause significant discomfort, pain, and limited mobility in the shoulder joint, impacting daily activities and overall quality of life.
In this comprehensive guide, we'll explore the connection between frozen shoulder and menopause, delving into the causes, symptoms, and effective solutions to manage this condition. By understanding the underlying factors and taking proactive steps, you can mitigate the effects of frozen shoulder and maintain an active, healthy lifestyle during this transitional phase.
What is Frozen Shoulder?
Frozen shoulder is a condition characterized by stiffness and pain in the shoulder joint, which can significantly restrict movement. It typically progresses through three distinct stages:
Stage 1: Freezing
During this initial phase, individuals may experience a gradual increase in shoulder pain, which can last for several weeks or months. Movement becomes increasingly limited as the pain intensifies, making it challenging to perform everyday activities.
Stage 2: Frozen
In this stage, the pain may begin to decrease, but the shoulder becomes stiffer, making it difficult to perform even simple tasks like reaching overhead or behind the back. This stage can last from several months to a year or more.
Stage 3: Thawing
The final stage involves a gradual return of motion in the shoulder, which can take several months to years. While pain may diminish, some stiffness may persist, and it may take time to regain full range of motion.

The Connection Between Menopause and Frozen Shoulder
While the exact cause of frozen shoulder is not fully understood, there are several factors that can contribute to its development, particularly during menopause.
Hormonal Changes
During menopause, women experience a significant drop in estrogen levels. Estrogen plays a crucial role in maintaining joint health and flexibility. The decline in this hormone can lead to increased joint stiffness and inflammation, making women more susceptible to conditions like frozen shoulder.
Age Factor
Frozen shoulder is more common in individuals aged 40 to 60, which coincides with the age range when many women enter menopause. Additionally, age-related changes in connective tissue can contribute to the onset of this condition.
Other Contributing Factors
Several other factors can exacerbate the risk of frozen shoulder during menopause:
Sedentary Lifestyle: With the physical changes that come with menopause, many women may become less active. A sedentary lifestyle can lead to muscle weakness and stiffness, increasing the likelihood of developing frozen shoulder.
Previous Shoulder Injuries: Women with a history of shoulder injuries or surgeries may find that menopause triggers or exacerbates frozen shoulder symptoms.
Underlying Health Conditions: Conditions such as diabetes, thyroid disorders, and cardiovascular diseases can increase the risk of frozen shoulder, particularly during menopause.
Symptoms of Frozen Shoulder
The symptoms of frozen shoulder can vary in severity, but typically include:
Pain: A dull or aching pain in the shoulder, often worsening at night or with movement.
Stiffness: Difficulty in moving the shoulder, especially when reaching overhead, behind the back, or performing daily activities.
Limited Range of Motion: A noticeable decrease in the ability to perform daily activities, such as dressing, reaching for objects, or carrying items.

Diagnosis of Frozen Shoulder
If you suspect you have frozen shoulder, it's essential to consult a healthcare professional for proper diagnosis and treatment. The diagnostic process typically involves:
Physical Examination: Your healthcare provider will assess the range of motion and pain levels in your shoulder joint.
Imaging Tests: X-rays or MRI scans may be used to rule out other conditions or identify any underlying issues contributing to your symptoms.
Treatment Options for Frozen Shoulder
Frozen shoulder can be managed through a combination of non-surgical and surgical treatments, depending on the severity of the condition and the individual's response to initial interventions.
Non-Surgical Treatments
Most cases of frozen shoulder can be managed without surgery. Here are some effective non-surgical treatment options:
Physical Therapy: Engaging in physical therapy can help restore movement and reduce pain. A physical therapist can design a personalized exercise program to improve flexibility, strength, and range of motion in the affected shoulder.
Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain and inflammation. In some cases, corticosteroid injections may be recommended to reduce inflammation and improve mobility.
Heat and Ice Therapy: Applying heat or ice to the shoulder can provide relief from pain and stiffness. Heat helps relax muscles, while ice reduces inflammation.
Surgical Treatments
If non-surgical treatments do not provide adequate relief, surgical options may be considered:
Manipulation Under Anesthesia: This procedure involves the doctor moving the shoulder while the patient is under anesthesia to help loosen the joint capsule and break up adhesions.
Arthroscopic Surgery: In severe cases, arthroscopic surgery may be performed to remove scar tissue and adhesions, allowing for improved range of motion.
Lifestyle Changes to Prevent Frozen Shoulder
While menopause can increase the risk of developing frozen shoulder, there are several lifestyle changes you can make to help prevent or manage this condition:
Staying Active
Maintaining an active lifestyle is crucial for preventing frozen shoulder, especially during menopause. Regular exercise can help maintain joint flexibility, muscle strength, and overall physical fitness. Here are some tips:
Regular Exercise: Incorporate a mix of strength training and flexibility exercises into your routine. Activities like yoga, Pilates, and swimming can improve overall joint health and mobility.
Stretching: Daily stretching can help maintain flexibility in the shoulder joint. Focus on gentle stretches that target the shoulder area, such as arm circles, pendulum swings, and cross-body stretches.
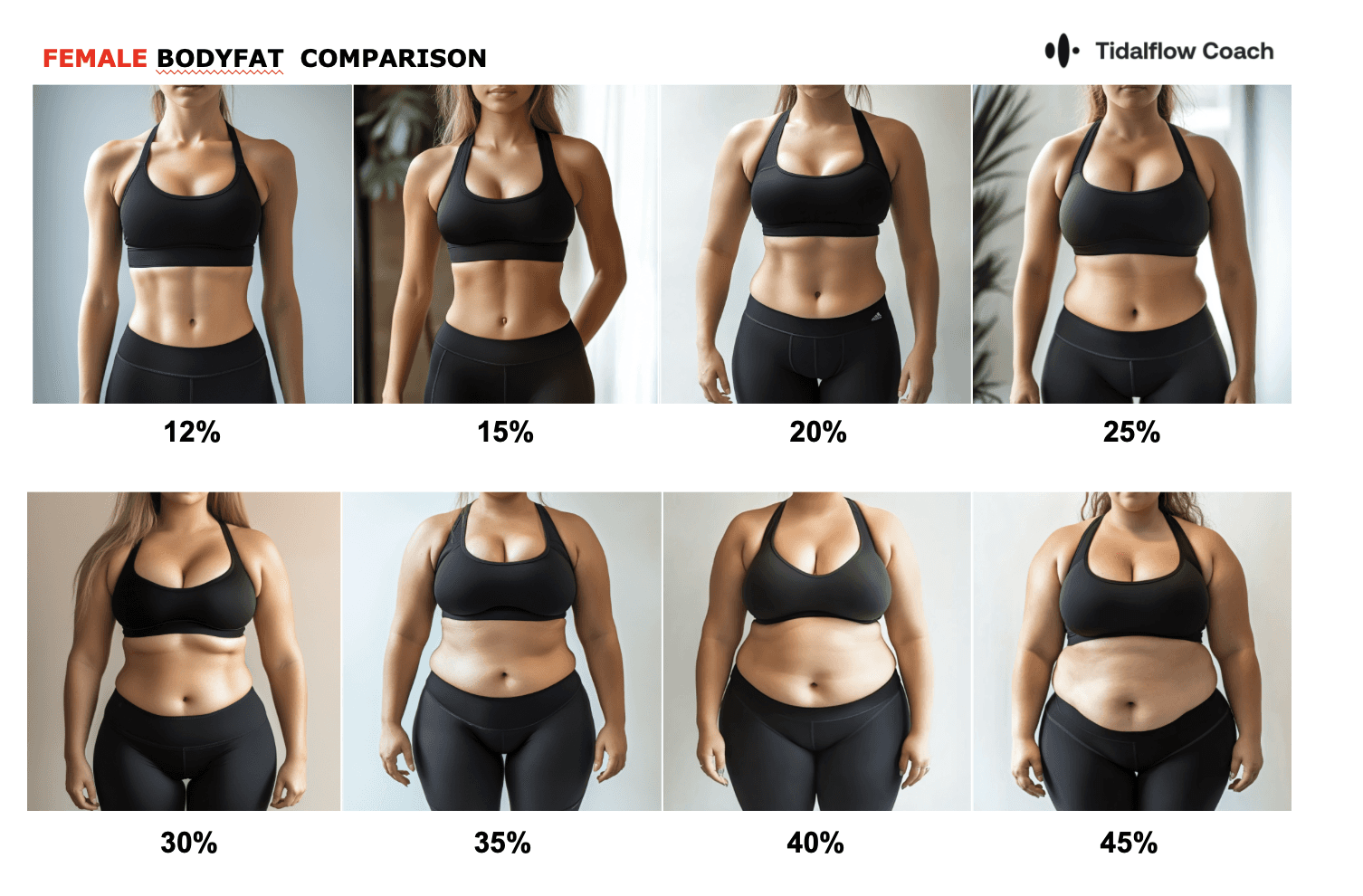
Weight Management: Maintaining a healthy weight can reduce stress on the joints. For personalized weight loss strategies, check out our guide on burning 400 calories daily.
Nutrition and Joint Health
Incorporating certain nutrients into your diet can support joint health and potentially reduce inflammation, which can be beneficial for managing frozen shoulder.
Anti-Inflammatory Diet: Eating a diet rich in anti-inflammatory foods can help reduce inflammation and support joint health. Consider incorporating foods like fatty fish (rich in omega-3 fatty acids), fruits and vegetables (rich in antioxidants), and whole grains.
Supplements: Consult with your healthcare provider about the potential benefits of supplements like glucosamine, chondroitin, and turmeric, which may help support joint health and reduce inflammation.

Seeking Professional Help
If you experience persistent shoulder pain, stiffness, or limited range of motion, it's essential to seek medical advice. A healthcare provider can help determine the best course of action tailored to your needs, which may include physical therapy, medication, or surgical intervention if necessary.
At Tidalflow, we understand the challenges that women face during menopause, including conditions like frozen shoulder. Our AI-powered personal training solutions are designed to help you stay active, manage your health, and maintain a high quality of life during this transitional phase. Explore our services today to find a program that works for you and take control of your wellness journey.
Conclusion
Frozen shoulder can be a challenging condition, especially for women navigating the changes of menopause. By understanding the connection between frozen shoulder and menopause, its causes, symptoms, and effective solutions, you can take proactive steps to manage this condition and maintain an active, healthy lifestyle. Remember, seeking professional help, staying active, and incorporating a nutrient-rich diet can all contribute to better joint health and overall well-being during this transitional phase.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice. Consult a healthcare provider for personalized recommendations.
You should not have to do it all on your own